1801006021 -short case
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
35 YR OlD MALE PATIENT , LORRY DRIVER BY OCCUPATION , RESIDENT OF ATTHAMPET ,CAME TO THE OPD WITH THE
C/O Pain abdomen since 10days,
yellowish discolouration of urine since 8 days
Distension of abdomen since 6 days
Bilateral lower limb swelling since 5 days .
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 10days ago and then developed,abdominal pain ,which was insidious in onset and gradually progressive ,which was of dragging type and diffuse, No aggravating factors but relieved on medication and reccured on stoping medication ,but not relieved on leaning forward .
Yellowish discolouration of urine since 8 days, NOT ASSOCIATED with any poor stream ,pyuria ,hematuria ,increased frequency , nocturia ,Burning micturition but decreased urine output present since 5days
Abdominal distension
and bilateral lower limbs edema since 6days,which were insidious in onset and gradually progressive, pitting type of edema over bilateral lower limbs,till knees
Pitting Type Of Edema :
Constipation since 5 days, Not associatied with passage of blood in stool /melena
PAST HISTORY:
No history of similar complaints in the past
K/C/O DIABETES MELLITUS ,which was diagnosed 5 months ago and started on ORAL HYPOGLYCEMIC DRUGS ( pt couldnt remember the drugs names )
N/K/C/O HTN , EPILEPSY ,CAD,CVA ,TB ,ASTHMA
PERSONAL HISTORY:
Sleep - Disturbed since 10days.
Diet - Mixed
Appetite - Disturbed since 6 days
Bowel and bladder movements : IRREGULAR ( decreased urine output and Stools not passed since 5 days )
Addictions : Alcoholic and chronic smoker since 10years
GENERAL EXAMINATION:
Patient is drowsy not coherent and not co operative, moderately built and nourished.
Vitals at presentation
Temp : Afebrile
BP: 110/80mmHg
PR: 86bpm
RR: 20cpm
SpO2 : 98%
Pallor - absent
Icterus - present -
Cyanosis:- absent
Clubbing - absent
Lymphadenopathy : absent
Edema : Present till knee level and of pitting type
PER ABDOMEN
Patient was examined after taking consent in a well lit room
ON INSPECTION
Abdomen is distended
umbilicus is inverted
Skin over abdomen is stretched and shiny
No visible pulsations
Engorged veins - Present
PALPATION :
all inspectory findings confirmed
No rise of temperature and tenderness
No guarding and rigidity
Liver and spleen are unable to palpate due to ascites.
PERCUSSION :
Shifting dullness - Present
Fluid thrills - Present
Puddle sign cannot be elicited ,as pt is not cooperative
AUSCULTATION :
Sluggish bowel sounds are heard
No bruits
CVS : S1 and S2 heard
no murmurs
CNS: No flapping tremors( Asterexis )
(Apraxia cannot be elicited as pt is not cooperative )
Apraxia Charting after 5 days of Hospital Stay :
RS : bilateral air entry is present
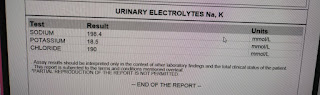
INVESTIGATIONS:
ASCITIC TAP DONE and fluid sent for analysis :
ASCITIC TAP DONE and fluid sent for analysis :
CT scan : Showing Calcifications:
CT scan : Showing Calcifications:
USG REPORT:
Enlarged liver with altered echotexture s/o CLD
gall bladder edema with sludge
Gross ascitis
Provisional Diagnosis :
Chronic liver disease 2° to alcohol intake with Type II DM
Alcohol dependence Syndrome
Chronic pancreatitis
MANAGEMENT:
) IV fluid NS 50 ml /hr
2) inj lasix 40mg IV /BD
3) T. Aldactone 50mg RT /OD
5) Syp . Lactulose 15ml RT /TID
6) Salt and fluid restriction ; Salt < 2gm /day , fluid < 1.5 lit /day
7) inj 3 amp KCL in 500ml NS over 5 hrs
8) Weight and abdominal girth daily
9) GRBS monitoring 2nd hrly
10) vitals monitoring 4th hrly
12) inj .Thiamine 200mg IV /BD
13) 3-4 egg whites /day
14) protein X powder 3-4 scoops in glass of milk RT/TID.
Follow up:-
Patient visited two times since December
Maintenance on
*Udiliv- 300
*Viboliv
*Thiamine
Abdominal distention and jaundice subsided.



























Comments
Post a Comment